Abstract
Introduction. For decades, the study of genomic alterations in Hodgkin lymphoma (HL) has been hampered by the low abundance of the malignant Hodgkin Reed-Sternberg (HRS) cells in HL lymph node biopsies. Laser microdissection or flow cytometric cell sorting allow the study of purified HRS cells, but the use of these applications is restricted to specialized research centers. We have recently demonstrated proof-of-principle that copy number aberrations (CNA) in HRS cells can be retrieved in circulating cell-free DNA (cfDNA) of HL patients (Vandenberghe et al., Lancet Haematol. 2015). Taking advantage of the presence of HRS cell-derived DNA (ctDNA) in plasma, the aim of this study was to catalogue CNA in HL in a large series of prospectively recruited HL patients.
Methods. We analyzed plasma collected from 177 patients (median age 29, range 3-86) with newly diagnosed HL. 60 cases were diagnosed at our institution, including all disease subtypes and stages, with a majority of nodular sclerosis. 118 patients were recruited in the context of the BREACH study, a multicentric Phase 2B study for unfavorable early classical HL (NCT02292979). After cfDNA extraction, samples were low-pass sequenced (0.1x coverage) and analyzed using ichorCNA, an algorithm that produces read depth-based log2 CNA profiles and quantifies the cfDNA tumor content.
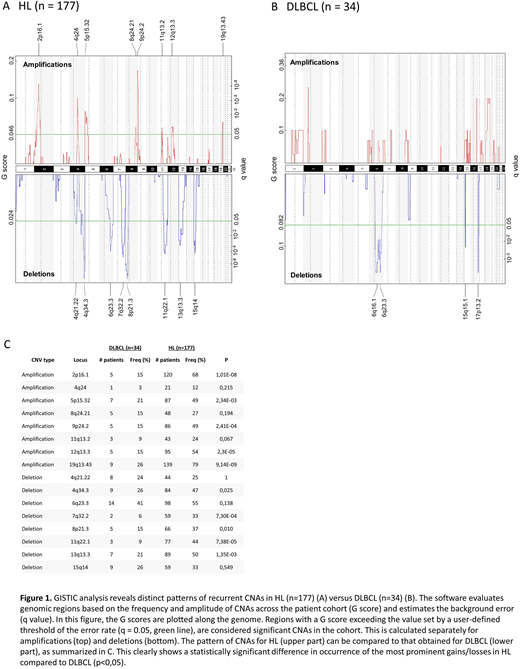
Results. At diagnosis, 86 % (152/177) of patients showed obvious genomic imbalances in cfDNA, in early-stage (85 % (131/155)) as well as in advanced cases (95 % (21/22)). Among the abnormal profiles, gains encompassing 2p16, 5p15, 9p24, 12q13 and 19q13 were the most frequent aberrations, occurring in 79 %, 53 %, 57 %, 63 % and 80 % respectively. Losses most frequently affected regions 4q34, 6q23, 11q22 and 13q13, in 53 %, 63 %, 49 % and 59 % of abnormal profiles respectively (fig. 1A). All these CNAs have been previously described with varying frequencies in smaller series of 10-53 patients, using arrayCGH or whole exome sequencing on microdissected HRS cells or even HRS cell-derived cell lines as input material. The observed pattern of CNAs is distinct from the pattern we observed in cfDNA obtained from other hematological malignances, e.g. multiple myeloma and diffuse large B-cell lymphoma (fig. 1B, C).
Analysis of follow-up cfDNA samples revealed that the majority of patients rapidly clear their profiles during the first two treatment cycles. Of 123 samples analysed at d15 of cycle 1, 89 samples (72 %) showed a normal profile without CNAs.This suggests a relationship between the fraction of ctDNA in cfDNA and the disease burden. However, we could not find a correlation between the ctDNA fraction as calculated by ichorCNA and the metabolic tumor volume as computed from PET/CT scans. This could be due to several factors, e.g. the small fraction of HRS cells in the metabolic tumor volume. We are currently investigating whether a correlation does exist between the HRS content in the lymph node biopsy and the ctDNA load.
Conclusions. In this largest study of CNA in HL to date, we provide a comprehensive catalogue of the types of CNAs, as well as their frequencies and patterns in HL. In this series of 177 patients, gains affecting 2p, 12q and 19q and loss of 6q and 13q emerge as the most commonly recurrent CNAs in HL, across all HL subtypes and stages. The data confirm and extend our previous findings that the majority of HL patients, including those with early-stage disease, have detectable CNAs in their cfDNA at diagnosis. We demonstrate a broad spectrum of aberrations, gains and losses, some of which recur at higher frequencies than gains of 9p24, harboring PD-L1. This warrants further studies on how these CNAs are implicated in the pathogenesis of HL. It further endorses the use of ctDNA as an alternative gateway to the genome of HRS cells, and as a substrate for the evaluation of early disease response.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal